Definition chronic, generally variable inflammatory disorder of the airways resulting in episodes of reversible hyper-responsive inf...
Definition
- chronic, generally variable inflammatory disorder of the airways resulting in episodes of reversible hyper-responsive inflammation and bronchospasm causing airflow obstruction
- paroxysmal or persistent symptoms such as dyspnea, chest tightness, wheezing, sputum production and/or cough
- associated with reversible airflow limitation and airway hyper-responsiveness to endogenous or exogenous stimuli
Epidemiology
- common (7-10% of adults), especially in children (10-15%)
- most children with asthma improve significantly in adolescence
- often family history of atopy (asthma, allergic rhinitis, eczema)
- occupational asthma
Etiology and Pathophysiology
- acute asthma: airway obstruction ---> V/Q mismatch ---> hypoxemia ---> increased ventilation ---> decreased PaCO2 ---> increased pH and muscle fatigue ---> decreased ventilation, increased PaCO2/decreased pH
Triggers
- URTIs, allergens (pet dander, house dusts, molds), irritants (cigarette smoke, air pollution), drugs (NSAIDs, beta-blockers), preservatives (sulphites, MSG), other (emotion/anxiety, cold air, exercise, GERD)
Signs and Symptoms
- tachypnea, wheezing, chest tightness, cough (especially nocturnal), sputum production
Important Signs and Symptoms
| Red Flags | Respiratory Distress |
| fatigue diminished expiratory effort cyanosis silent chest decreased LOC | nasal flaring, tracheal tug inability to speak accessory muscle use, intercostal indrawing pulsus paradoxus |
Risk Factors Indicating Poor Asthma Control
| Previous Non-Fatal Episodes | Ominous Signs and Symptoms |
| loss of consciousness during asthma attack frequent ER visits prior intubation ICU admission | night time symptoms >1 night/week silent chest FEV1 or PEF (peak expiratory flow) <60% limited activities of daily living use of beta2 agonists >3 times/day |
Criteria for determining whether asthma is well controlled
- daytime symptoms <4 days/wk
- no asthma-related absence from work/school
- night-time symptoms, <1 night/wk
- beta-2 agonist use <4 times/wk
- normal physical activity
- FEV1 or PEF >90% of personal best
- mild, infrequent exacerbations
- PEF diurnal variation <10-15%
Investigations
- O2 saturation
- ABGs
- decreased PaO2 during attack (V/Q mismatch)
- decreased PaCO2 in mild asthma due to hyperventilation
- normal or increased PaCO2 ominous as patient is no longer able to hyperventilate (worsened airway obstruction or respiratory muscle fatigue)
- PFTs (may not be possible during severe attack, do when stable)
- spirometry: increase in FEV1 >12% with beta2-agonist, or >20% with 10-14 days of steroids, or >20% spontaneous variability
- provocation testing: decrease in FEV1 >20% with methacholine challenge
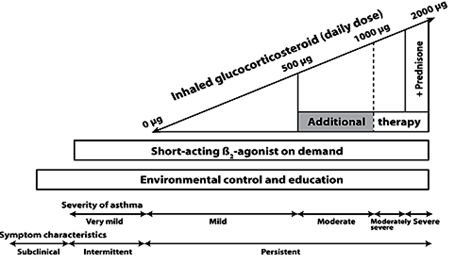
Treatment
- environmental control: avoid relevant triggers
- patient education: features of the disease, goals of treatment, self-monitoring
- pharmacological therapy:
- symptomatic relief in acute episodes: short-acting beta2-agonist, anticholinergic bronchodilators, oral steroids, addition of a long acting beta2-agonist
- long-term prevention of acute episodes: inhaled/oral corticosteroids, anti-allergic agent, long-acting beta2-agonist, methylxanthine, leukotriene receptor antagonists (LTRA)
Clinical Pearl
Central cyanosis is not detectable until the SaO2 is <85%.
It is more easily detected in polycythemia and less readily detectable in anemia.
Asthma Triad
asthma
ASA/NSAID sensitivity
nasal polyps
Guidelines for Asthma Management
Eemergency Management of Asthma
- inhaled beta2-agonist first line (MDI route and spacer device recommended)
- add anticholinergic therapy
- ketamine and succinylcholine for rapid sequence intubation in life-threatening cases
- SC/IV adrenaline, IV salbutamol if unresponsive
- all patients admitted to ER for asthma exacerbations should be considered for corticosteroid therapy at discharge
Clinical Pearl
Remember to step down therapy to lowest doses which control symptoms/signs of bronchoconstriction.
Medical Mnemonics
Beta-1 vs Beta-2 receptor location
"You have 1 heart and 2 lungs":
Beta-1 are therefore primarily on heart.
Beta-2 primarily on lungs.
Zafirlukast, Montelukast, Cinalukast: mechanism, usage
"Zafir-luk-ast, Monte-luk-ast, Cina-luk-ast":
· Anti-Lukotrienes for Asthma.
· Dazzle your oral examiner: Zafirlukast antagonizes leukotriene-4.
Asthma drugs: leukotriene inhibitor action
zAfirlukast: Antagonist of lipoxygenase
zIlueton: Inhibitor of LT receptor