systemic venous return re-enters systemic circulation directly most prominent feature is cyanosis (O2 sat < 75%) differentiate...
- systemic venous return re-enters systemic circulation directly
- most prominent feature is cyanosis (O2 sat < 75%)
- differentiate between cardiac and other causes of cyanosis with hypoxia test
- survival depends on mixing via shunts (e.g. ASD, VSD, PDA)
Transposition of the Great Arteries
- most common cardiac lesion in the cyanotic newborn
- aortic root arises anteriorly from the right ventricle and the main pulmonary artery arises posteriorly from left ventricle, resulting in parallel pulmonary and systemic circulations
- newborn presents with progressive cyanosis unresponsive to oxygen therapy as the ductus arteriosus closes and mixing between the two circulations diminishs; severe hypoxemia, acidosis, and death can occur rapidly
- if VSD present, cyanosis is not prominent, infant presents with CHF
after a few weeks of life - Murmur: none or grade II/VI SEM
- ECG: RAD, RVH
- CXR: egg-shaped heart with narrow mediastinum ("egg on a string")
Management:
- prostaglandin E1 infusion to keep ductus open
- balloon atrial septostomy with catheter
- surgical correction: arterial switch procedure
Tetralogy of Fallot
- most common cyanotic heart defect
- 10% of all congenital heart defects,
- beyond infancy embryologically a single defect with hypoplasia of the conus causing:
- VSD
- RV outflow tract obstruction (RVOTO)
- overriding aorta
- RVH
- direction and degree of shunt are functions of the relative outflow resistance
- infants may initially have a left to right shunt and therefore are not cyanotic but the RVOTO is progressive, resulting in increasing right to left shunting with hypoxemia and cyanosis
- “TET” spells
- caused by increased right to left shunting due to exercise or crying which decreases systemic resistance
- paroxysm of rapid and deep breathing, irritability and crying
- increased cyanosis and decreased intensity of murmur
- peak incidence at 2-4 months of age
- if severe may lead to seizures, loss of consciousness, death (rare)
- management: oxygen, knee-chest position, morphine sulfate, propanolol
- murmur: single loud S2 due to severe pulmonic stenosis
- ECG: right axis deviation, RVH
- CXR: boot shaped heart, decreased pulmonary vasculature, right aortic arch
- management: surgical repair including closure of VSD and widening of RVOTO
Clinical Pearl : Characteristic Chest X-Ray Findings in Congenital Heart Disease


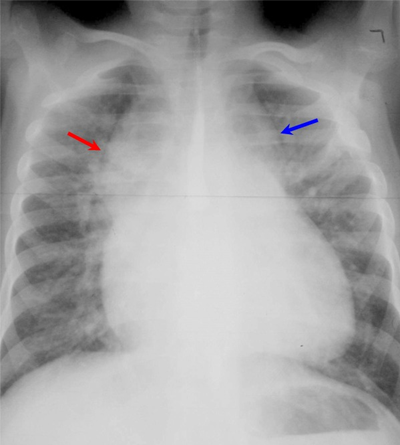
The heart has a "snowman shape." The pulmonary veins drain into an enlarged vertical vein (blue arrow) which in turn drains into the brachiocephalic vein and then to the superior vena cava (red arrow). The vasculature is shunt vasculature.





